Paralisis Spastik Dan Flaksid Pada Cacing
In Stroke Physical Therapy plays an important role in the process of rehabilitation. As a part of the interdisciplinary team, work in concert with the managing doctor and other rehabilitation specialists to provide stroke patients with a comprehensive rehabilitation program. The stroke physical therapy rehabilitation program involves a dynamic process of assessment, goal-setting, treatment and evaluation; its coverage spans from the acute stage, through the rehabilitation stage, to the community stage.The whole rehabilitation program is predicated on two general components.
The first includes preventive measure targeted at maintaining physical integrity and minimizing complications that will prevent or prolong functional return. These measures should begin immediately post stroke and continue as long as necessary. The second component is restorative treatment aimed at promoting functional recovery.
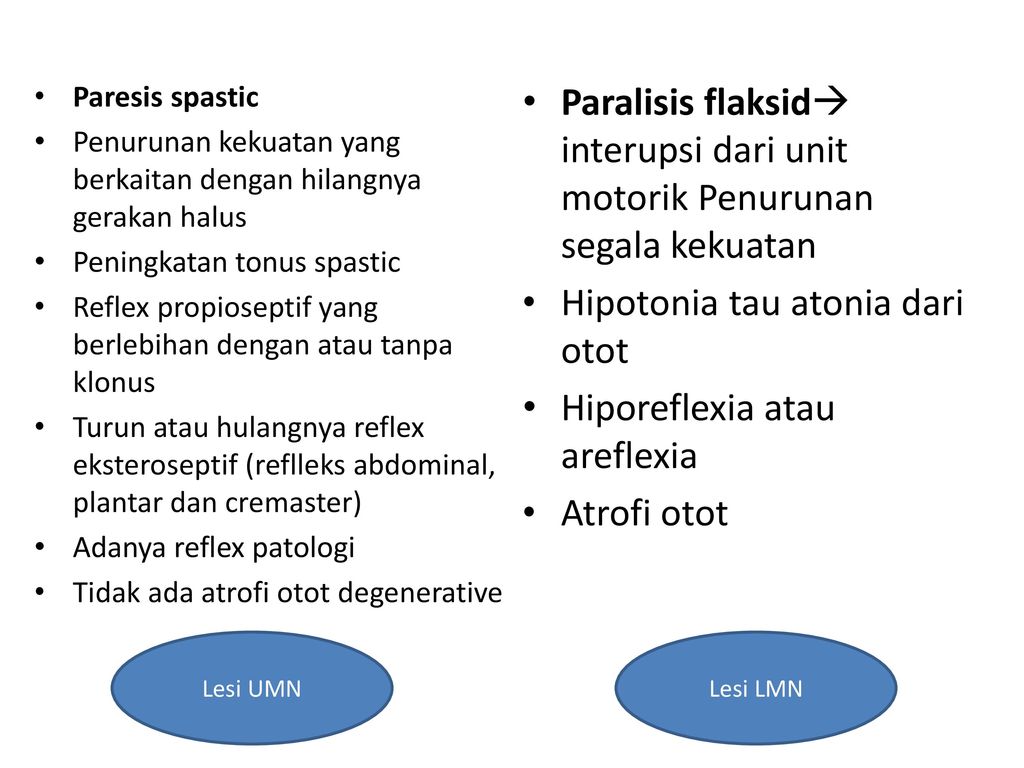
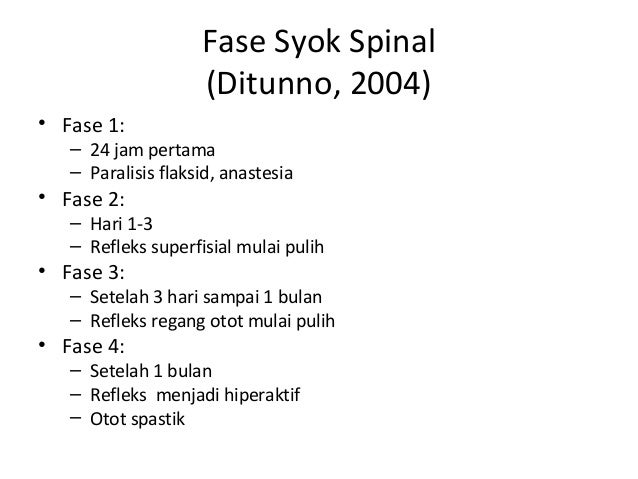
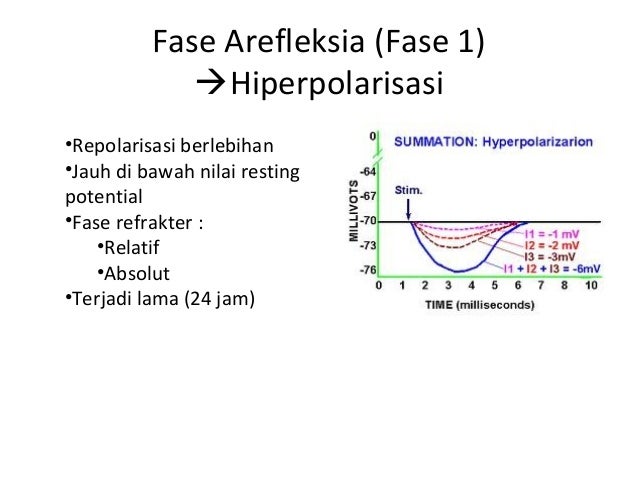
Kelumpuhan Flaccid vs. Spastic Kelumpuhan adalah kondisi yang terkait dengan hilangnya fungsi otot. Kelumpuhan ini disebabkan oleh kegagalan sistem saraf. Kegagalan sistem saraf dapat terjadi karena berbagai alasan seperti trauma, polio, botulisme dll. Kelumpuhan lunak dan kelumpuhan spastik dapat dianggap sebagai bentuk kelumpuhan. Artinya pada anak cerebral palsy terdapat dua atau lebih kelainan. Misalnya spastik dan athetosis, atau spastik dan rigid, atau spastik dan ataksia. Kecacatan tersebut tergantung pada kerusakan yang terjadi di otak. Letak kerusakan jenis ini di daerah pyramidal dan extrapyramidal. Apabila kerusakan terjadi pada pyramidal, kelainannya berbentuk.
This phase should begin as soon as the patient is medically and neurologically stable and has the cognitive and physical ability to participate actively in a rehabilitation program. In brief, the aims of physical therapy interventions are to promote motor recovery, optimize sensory functions, enhance functional independence, and prevent secondary complications. Goals of Physical therapyManagement of stroke patients begins as the acute care during acute hospitalization and continues as rehabilitative care as soon as patient’s medical & status has stabilized. Moreover, community reintegration of patients continues during the community care stage.1. Acute CareAims:1) Prevent recurrent stroke 2) Monitor vital signs, dysphasia adequate nutrition, bladder & bowel function. 3) Prevent complications 4) Mobilize the patient 5) Encourage resumption of self-care activities 6) Provide emotional support & education for patient & family 7)Screen for rehabilitation and choice of settings2. Rehabilitation careAims:1) Set rehabilitation goals; develop rehabilitation plan and monitor progress 2) Manage sensori-motor deficits 3) Improve functional mobility & independence 4) Prevent & treat complications 5) Monitor functional health conditions 6) Discharge planning (safe residence recommendation, patient & care givers education & continuity of care) 7) Community – reintegration3.
Community careAims:1) Assist patient to reintegrate into community 2) Enhance family and caregivers functioning 3) Co-ordinate continuity of patient care 4) Promote health and safety and prevent further hospitalization 5) Give advice on community supports, valued activities and vocational reintegrate. Stroke Physical Therapy assessment includesa) Patient characteristics. Demographics (age, gender). History of illness. Prior activity level (low to very high). Prior socialization (isolated to outgoing).
Expectations regarding stroke outcomes and need for assistance.b) Family and caregiver characteristics. Members of household and relationship to patient. Other potential caregivers. Capacity to provide physical, emotional, instrumental support.c) Impairmentse.g. Speech, seeing, muscle strength, balance, and co-ordination.d) Activitiese.g. Communication, movement, use of and technical aids.e) Participatione.g.
Mobility, personal maintenance, social relationships, work, leisure, hobby, economic lifef) Environment factorse.g. Personal support and assistance, social and economic institutions, physical environment such as access to building and key facilities within living quarters, safety considerations, access to resources and activities in community.Special considerationShoulder assessmentsubluxation and pain is a major and frequent complication in patients with hemiplegia. (Joynt, 1992; Grossen-Sils, and Schenkman, 1985). As many as 80% of patients with cerebrovascular accident has been reported to show shoulder subluxation. Clinical examination of shoulder should include thorough evaluation of pain, range of movement, motor control, and shoulder subluxation.Setting rehabilitation goalsIn Stroke Physical Therapy both short-term and long- term goals need to be realistic in terms of current levels of disability and the potential for recovery. Goals should be mutually agreed to by the patient, family, and rehabilitation team and should be documented in the medical record in explicit, measurable terms.Developing the rehabilitation management planIn Stroke Physical Therapy the rehabilitation management plan should indicate the specific treatments planned and their sequence, intensity, frequency, and expected duration. Measures to prevent complications of stroke and recurrent strokes should be continued.
Stroke Physical Therapy Interventions (1). Improving motor controla.Neurofacilitatory TechniquesIn Stroke Physical Therapy these therapeutic interventions use sensory stimuli (e.g. Quick stretch, brushing, reflex stimulation and associated reactions),which are based on neurological theories, to facilitate movement in patients following stroke (Duncan,1997). The following are the different approaches: -i.BobathBerta & Karel Bobath’s approach focuses to control responses from damaged postural reflex mechanism. Emphasis is placed on affected inputs facilitation and normal movement patterns (Bobath, 1990).ii.BrunnstromBrunnstrom approach is one form of neurological exercise therapy in the rehabilitation of stroke patients. The relative effectiveness of Neuro-developmental treatment (N.D.T.) versus the Brunnstrom method was studied by Wagenaar and colleagues (1990) from the perspective of the functional recovery of stroke patients.
The result of this study showed no clear differences in the effectiveness between the two methods within the framework of functional recovery.iii.RoodEmphasise the use of activities in developmental sequences, sensation stimulation and muscle work classification. Cutaneous stimuli such as icing, tapping and brushing are employed to facilitate activities.iv.
Proprioceptive neuromuscular facilitation (PNF)Developed by Knott and Voss, they advocated the use of peripheral inputs as stretch and resisted movement to reinforce existing motor response. Total patterns of movement are used in treatment and are followed in a developmental sequence.It was shown that the commutative effect of is beneficial to stroke patient (Wong, 1994). Comparing the effectiveness of PNF, Bobath approach and traditional exercise, Dickstein et al (1986)demonstrated that no one approach is superior to the rest of the others (AHCPR, 1995).b. Learning theory approachi. Conductive educationIn Stroke Physical Therapy, Conductive education is one of the methods in treating neurological conditions including hemiplegic patients. Cotton and Kinsman (1984) demonstrated a neuropsychological approach using the concept of CE for adult hemiplegia. The patient is taught how to guide his movements towards each task-part of the task by using his own speech - rhythmical intention.ii.
Motor relearning theoryCarr & Shepherd, both are Australian physiotherapists, developed this approach in 1980. It emphasises the practice of functional tasks and importance of relearning real-life activities for patients. Principles of learning and biomechanical analysis of movements and tasks are important. (Carr and Shepherd, 1987)There is no evidence adequately supporting the superiority of one type of exercise approaches over another. However, the aim of therapeutic approach is to increase physical independence and to facilitate the motor control of skill acquisition and there is strong evidence to support the effect of rehabilitation in terms of improved functional independence and reduced mortality.c. Functional electrical stimulation (FES)FES is a modality that applied a short burst of electrical current to the hemiplegic muscle or nerve.
In Stroke Physical Therapy, FES has been demonstrated to be beneficial to restore, and reduction of hemiplegic shoulder pain and subluxation. It is concluded that FES can enhance the upper extremity motor recovery of acute stroke patient (Chae et al., 1998; Faghri et al., 1994; Francisco, 1998). Alfieri (1982) and Levin et al (1992) suggested that FES could reduce spasticity in stroke patient. A recent meta- analysis of randomized controlled trial study showed that FES improves motor strength (Glanz 1996). Best cpu temperature for mac. Study by Faghri et al (1994) have identified that FES can significantly improve arm function, electromygraphic activity of posterior deltoid, range of motion and reduction of severity of subluxation and pain of hemiplegic shoulder.d. BiofeedbackBiofeedback is a modality that facilitates the cognizant of electromyographic activity in selected muscle or awareness of joint position sense via visual or auditory cues.
In Stroke Physical Therapy the result of studies in biofeedback is controversial. A meta-analysis of 8 randomized controlled trials of biofeedback therapy demonstrated that electromyographic biofeedback could improve motor function in stroke patient (Schleenbaker, 1993). Another meta-analysis study on EMG has showed that EMG biofeedbcak is superior to conventional therapy alone for improving ankle dorsiflexion muscle strength (Moreland et al., 1998.
Erbil and co-workers (1996) showed that biofeedback could improve earlier postural control to improve impaired sitting balance. Conflicting meta-analysis study by Glanz et al (1995) showing that biofeedback was not efficacious in improving range of motion in ankle and shoulder in stroke patient. Moreland (1994) conducted another meta-analysis concluded that EMG biofeedback alone or with conventional therapy did not superior to conventional physical therapy in improving upper- extremity function in adult stroke patient.
(2) Hemiplegic shoulder managementShoulder subluxation and of the affected arm is not uncommon in at least 30% of all patient after stroke (RCP, 1998),whereas subluxation is found in 80% of stroke patients (Najenson et al., 1971). It is associated with severity of disability and is common in patients in rehabilitation setting. Suggested interventions are as follows:a) ExerciseActive weight bearing exercise can be used as a means of improving motor control of the affected arm; introducing and grading tactile, proprioceptive, and kinesthetic stimulation; and preventing edema and pain.
In Stroke Physical Therapy, Upper extremity weight bearing can be used to lengthen or inhibit tight or spastic muscles while simultaneously facilitating muscles that are not active (Donatelli, 1991). According to Robert (1992), the amount of shoulder pain in hemipelgia was related most to loss of motion. He advocated that the provision of (caution to avoid imprigement) as treatment as early as possible.b) Functional electrical stimulationFunctional electrical stimulation (FES) is an increasingly popular treatment for the hemiplegic stroke patient. It has been applied in stroke physical therapy for the treatment of shoulder subluxation (Faghri et al.,1994), spasticity (Stefanovska et al., 1991) and functionally, for the restoration of function in the upper and lower limb (Kralji et al., 1993). In Stroke Physical Therapy, Electrical stimulation is effective in reducing pain and severity of subluxation, and possibly in facilitating recovery of arm function (Faghri, et al., 1994; Linn, et al., 1999).c) Positioning & proper handlingIn Stroke Physical Therapy, proper positioning and handling of hemiplegic shoulder, whenever in bed, sitting and standing or during lifting, can prevent shoulder injury is recommended in the AHCPR & SIGN guidelines for stroke rehabilitation.
In Stroke Physical Therapy, positioning can be therapeutic for tone control and neuro-facilitation of stroke patients (Davies, 1991). Braus et al 94 found shoulder hand syndrome reduced from 27% to 8% by instruction to every one including family on handling technique.d) Neuro-facilitatione) Passive limb physiotherapyMaintenance of full pain-free range of movement without traumatizing the joint and the structures can be carried out. In Stroke Physical Therapy, at no time should pain in or around the shoulder joint be produced during treatment. (Davies, 1991).f) Pain relief physiotherapyPassive mobilisation as described by Maitland, can be useful in gaining relief of pain and range of movement (Davies, 1991). In Stroke Physical Therapy other treatment modalities such as thermal, electrical, cryotherapy etc. Can be applied for shoulder pains of musculoskeletal in nature.g) Reciprocal pulley The use of reciprocal pulley appears to increase risk of developing shoulder pain in stroke patients. It is not related to the presence of subluxation or to muscle strength.
(Kumar et al., 1990)h) SlingIn Stroke Physical Therapy the use of sling is controversial. No shoulder support will correct glenohumeral joint subluxation.
However, it may prevent the flaccid arm from hanging against the body during functional activities, thus decreasing shoulder joint pain. They also help to relieve downward traction on the shoulder capsule caused by the weight of the arm (Hurd, Farrell, and Waylonis, 1974; Donatelli,1991).
(3) Limb physiotherapyLimb physiotherapy/Stroke Physical Therapy includes passive, assisted-active and active range-of-motion exercise for the hemiplegic limbs. This can be an effective management for prevention of limb contractures and spasticity and is recommended within AHCPR (1995).
Self-assisted limb exercise is effective for reducing spasticity and shoulder protection (Davis, 1991). Adams and coworkers (1994) recommended passive full-range-of-motion exercise for parlysed limb for potential reduction of complication for stroke patients (4)In Stroke Physical Therapy, evidence shows that both cough and forced expiratory technique (FET) can eliminate induced radio aerosol particles in lung field. Directed coughing and FET can be used as a technique for bronchial hygiene clearance in stroke patient. (5) PositioningIn Stroke Physical Therapy consistent “reflex-inhibitory” patterns of posture in resting is encouraged to discourage physical complication of stroke and to improve recovery (Bobath, 1990).Meanwhile, therapeutic positioning is a widely advocated strategy to discourage the development of abnormal tone, contractures, pain and respiratory complications. It is an important element in maximizing the patient's functional gains and quality of life. (6) Tone managementA goal of Stroke Physical Therapy interventions has been to “normalize tone to normalize movement.” Therapy modalities for reducing tone include, prolonged stretching, passive manipulation by therapists, weight bearing, ice, contraction of muscles antagonistic to spastic muscles, splinting, and casting.
Research on tone-reducing techniques has been hampered by the inadequacies of methods to measure spasticity (Knutsson and Martensson, 1980) and the uncertainty about the relationship between spasticity and volitional motor control (Knutsson and Martensson, 1980; Sahrmann and Norton, 1977). Manual stretch of finger muscles, pressure splints, and dantrolene sodium do not produce apparent long-term improvement in motor control (Carey, 1990; Katrak, Cole, Poulus, and McCauley, 1992; Poole, Whitney, Hangeland, and Baker, 1990). Dorsal resting hand splints reduced spasticity more than volar splints, but the effect on motor control is uncertain (Charait, 1968) while TENS stimulation showed improvement for chronic spasticity of lower extremities (Hui-Chan and Levin, 1992). (7) Sensory re-educationBobath and other therapy approaches recommend the use of sensory stimulation to promote sensory recovery of stroke patients. (8) Balance retrainingRe-establishment of balance function in patients following stroke has been advocated as an essential component in the practice of stroke physical therapy (Nichols, 1997). Some studies of patients with hemiparesis revealed that these patients have greater amount of postural sway, asymmetry with greater weight on the non-paretic leg, and a decreased ability to move within a weight-bearing posture (Dickstein, Nissan, Pillar, and Scheer, 1984; Horak, Esselman, Anderson, and Lynch, 1984). Meanwhile, research has demonstrated moderate relationships between balance function and parameters such as gait speed, independence, wheelchair mobility, reaching, as well as dressing (Dickstein et al., 1984; Horak et al., 1984; Bohannon, 1987; Fishman, Nichols, Colby, and Sachs, 1996; Liston and Brouwer, 1996; Nichols, Miller, Colby and Pease, 1996).
Some tenable support on the effectiveness of treatment of disturbed balance can be found in studies comparing effects of balance retraining plus physiotherapy treatment and physiotherapy treatment alone. (9) Fall preventionIn Stroke Physical Therapy, are one of the most frequent complications( Dromerick and Reading, 1994), and the consequences of which are likely to have a negative effect on the rehabilitation process and its outcome. According to the systematic review of the Cochrane Library (1999), which evaluatedthe effectiveness of several fall prevention interventions in the, there was significant protection against falling from interventions which targeted multiple, identified, risk factors in individual patients.
The same is true for interventions which focused on behavioural interventions targeting environmental hazards plus other risk factors (10) Gait re-educationRecovery of independent mobility is an important goal for the immobile patient, and much therapy is devoted to gait-reeducation. Bobath assume abnormal postural reflex activity is caused of dysfunction so gait training involved tone normalization and preparatory activity for gait activity. In contrast Carr and Shepherd advocates task-related training with methods to increase strength, coordination and flexible MS system to develop skill in walking while Treadmill training combined with use of suspension tube.
Some patient’s body weight can effective in regaining walking ability, when used as an adjunct to convention therapy 3 months after active training (Visintin et al., 1998; Wall and Tunbal 1987; Richards et al., 1993). (11) Functional Mobility TrainingTo handle through the functional limitations of stroke patients, functional tasks are taught to them based on movement analysis principles. In Stroke Physical Therapy these tasks include bridging, rolling to sit to stand and vice versa, transfer skills, walking and stairing etc (Mak et al., 2000).Published studies report that many patients improve during rehabilitation. The strongest evidence of benefit is from studies that have enrolled patients with chronic deficits or have included a no-treatment control group (Wade et al., 1992; Smith and Ashburn et al., 1981).Meanwhile, early mobilization helps prevent compilations e.g. DVT, skin breakdown contracture and pneumonia. Evidence have shown better orthrostatic tolerance (Asberg, 1989) and earlier ambulation (Hayes and Carroll, 1986). (12) Upper limb trainingBy 3 months poststroke, approximately 37% of the individuals continues to have decreased upper extremities (UE) function.
Recovery of UE function lags behind that of the lower extremities because of the more complex motor skill required of the UE in daily life tasks. That means many individuals who have a stroke are at risk for lowered quality of life.Many approaches to the physical rehabilitation of adults post-stroke exist that attempt to maximize motor skill recovery. However the literature does not support the efficacy of any single approach. The followings are the current approaches to motor rehabilitation of the UE.a) Facilitation modelsThey are the most common methods of intervention for the deficits in UE motor skills including Bobath, proprioceptive neuromuscular facilitation, Brunnstrom’s movement therapy and Rood’s sensorimotor approach.
There is some evidence that practice based on the facilitation models can result in improved motor control of UE ( Dickstein et al,1986, Grade A; Wagenaar et al, 1990 ). However, intervention based on the facilitation models has not been effective in restoring the fine hand coordination required for the performance of actions ( Kraft, Fitts & Hammond, 1992; Butefisch et al, 1995 ).b) Functional electric stimulationIn Stroke Physical Therapy, Functional electric stimulation (FES) can be effective in increasing the electric activity of muscles or increased active range of motion in individuals with stroke ( Dimitrijevic et al., 1996; Fields, 1987; Faghri et al., 1994,; Kraft, Fitts and Hammond, 1992 ). Some evidence shown that FES may be more effective than facilitation approaches ( Bowman, Baker and Waters, 1979; Hummelsheim, Maier-Loth and Eickhof, 1997 ).c) Electromyographic biofeedbackIn Stroke Physical Therapy, biofeedback can contribute to improvements in motor control at the neuromuscular and movement levels ( Kraft, Fitts and Hammond, 1992; Moreland and Thomson, 1994; Wissel et al., 1989; Wolf and Binder-MacLoed, 1983; Wolf, LeCraw and Barton,1989; Wolf et al., 1994 ). Some studies have shown improvments in the ability to perform actions during post-testing after biofeedback training ( Wissel et al.,1989; Wolf and Binder-MacLoed, 1983; Moreland and Thomson, 1994).
However, the ability to generalize these skills and incorporate them into daily life is not measured.d) Constraint-induced therapyConstraint-Induced (CI) therapy was designed to overcome the learned nonuse of the affected UE. In the most extreme form of CI therapy, individual post-stroke are prevented from using the less affected UE by keeping it in a splint and sling for at least 90% of their waking hours. Studies have found that the most extreme of CI therapy can effect rapid improvement in UE motor skill ( Nudo et al., 1996; Taub and Wolf, 1997; Taub et al., 1993; Wolf et al., 1989 ) and that is retained for at least as long as 2 years ( Taub and Wolf, 1997 ). However, CI therapy, currently are effective only in those with distal voluntary movement ( Taub and Wolf, 1997 ). (13) Mobility appliances and equipmentSmall changes in an individual's local 'environment' can greatly increase independence, use of a wheelchair or walking stick. However, little research has been done for these 'treatments'. It is acknowledged that walking aids and mobility appliances may benefit selected patients.Tyson and Ashburn (1994) showed that walking aids had effect in poor walkers - a benefical effect on gait (Level of evidence = III, Recommendation = Grade B).
Lu and coworkers (1997) concluded that wrist crease stick is better than stick measured to greater trochanter. (Level of evidence = IIb, Recommendation = Grade A (14) AcupunctureThe World Health Organisation (WHO) has listed acupuncture as a possible treatment for pariesis after stroke. Studies had sown its beneficial effects in strike rehabilitation.Chen et al.
(1990) had performed a controlled clinical trial of acupuncture in 108 stroke patients. They stated that the total effective rate of increasing average muscle power by at least one grade was 83.3% in the acupuncture group compared with the controlled group which was 63.4% (p.
Paralysis is a loss of muscle function in part of your body. It can be localized or generalized, partial or complete, and temporary or permanent. Paralysis can affect any part of your body at any time in your life. If you experience it, you probably won’t feel pain in the affected areas.A treatment plan and outlook for the condition will depend on the underlying cause of paralysis, as well as symptoms experienced.
Technological innovations and therapeutic interventions may help you maintain your independence and quality of life. Doctors can classify paralysis in many different ways: LocationLocalized paralysis affects only one part of your body, such as your face or hand.Generalized paralysis is a group of conditions that affect multiple body parts. The types include:. monoplegia, which affects only one arm or leg. hemiplegia, which affects one arm and one leg on the same side of your body. paraplegia, which affects both of your legs. quadriplegia, or tetraplegia, which affects both of your arms and both of your legsSeverityIf you have partial paralysis, you’ll have some control over the muscles in the affected body parts.
If you have complete paralysis, you’ll have no control over the muscles in the affected areas. DurationYour paralysis may be temporary. For example, is a condition that can cause temporary paralysis of your face. Strokes can also temporarily paralyze one side of your body. With time and treatment, you may regain some or all of your feeling and coordination.In other cases, your paralysis may be permanent. Flaccid or spasticFlaccid paralysis causes your muscles to shrink and become flabby.
It results in muscle weakness. Spastic paralysis involves tight and hard muscles. It can cause your muscles to twitch uncontrollably, or spasm. Diagnosing paralysis is often easy, especially when your loss of muscle function is obvious. For internal body parts where paralysis is more difficult to identify, your doctor may use, or other imaging studies.If you experience a spinal cord injury, your doctor may use myelography to assess your condition.
In this procedure, they’ll insert a special dye into the nerves in your spinal cord. This will help them see your nerves more clearly on X-rays. They may also perform an electromyography. In this procedure, they’ll use sensors to measure electrical activity in your muscles.
A treatment plan will depend on the underlying cause of the paralysis, as well the symptoms experienced. For example, a doctor may prescribe:. surgery or possible amputation. physical therapy. occupational therapy. mobility aids, such as wheelchairs, braces, mobile scooters, or other devices. medications, such as Botox or muscle relaxers, if you have spastic paralysisIn many cases, paralysis isn’t curable.
But a healthcare team can recommend a variety of treatments, tools, and strategies to help manage symptoms. Many people with paralysis never regain mobility or sensation in the affected areas of their bodies. But even if a person’s paralysis isn’t curable, their healthcare team can recommend assistive technologies, therapeutic interventions, or other strategies to help improve quality of life.For example, special braces and electronic mobility devices may allow independent movement. Occupational therapists and other professionals can help modify the following to suit a patient’s abilities and needs:. clothes. home.
Paralisis Spastik Dan Flaksid Pada Cacing En
car. workplaceA doctor may also recommend lifestyle changes, medications, surgery, or other treatments to help manage potential complications.If you’re seeking treatment for paralysis, ask your doctor for more information about your specific diagnosis, treatment plan, and long-term outlook.
Blog
- Fallout 4 Winter Overhaul
- Pak Vs Aus Live Odi
- Battle For Middle Earth 2 Walkthrough
- Trimble Business Center 5.0 Crack
- Contoh Program C Menggunakan Fungsi Dan Prosedur
- Windows Has Recovered From An Unexpected Shutdown
- Pc Fallout 4 Cheats
- Mass Effect Heavy Armor
- Capello Dvd Player Manual
- Wow Unit Fram Addons
- What Does Lock The Taskbar Mean Windows 10
- Sublimetext Pros And Cons
- Disney Princess My Fairytale Adventure Pc Download
- Silent Hunter 4 Battle Of Midway
- Dien Dan Oppo A3s
- Gulperi Ep 10 Subtitrat In Romana
- Serial Windows 7 Ultimate 64 Bits Valido
- Blue Light Filter For Pc
- Aspire E 14 Usb Driver