What Does A Ub 92 Vs Hcfa 1500 Form Look Like
Individual provider claims are billed on the CMS 1500 form. All hospital (or institutional) claims are billed on the UB 04 claim form.Like the CMS 1500 claim form, an inpatient hospital coder fills out the UB04 form with the procedures and charges from the patient visit.
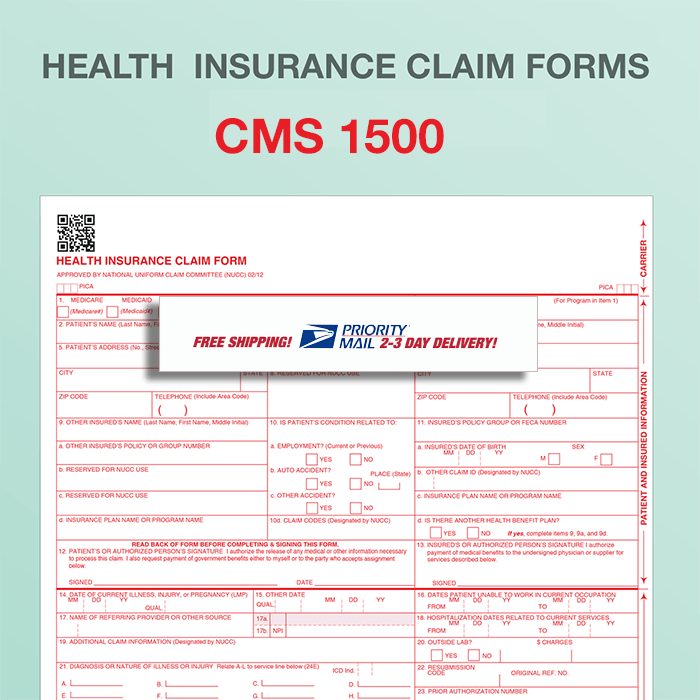
Making sense of Medicare paperwork, including the HCFA 1500 claim form, can be difficult. For that reason, here are some tips and a sample form to assist you. Please note that the lettered items on this page refer to letters printed on the sample form. Printed in the upper left-hand corner of your HCFA 1500 claim form are the name. CMS-1500 Form Requirements Item Number 19 Instructions Do not enter a space, hyphen or other separator between the qualifier code and the number. The taxonomy code is designated by the provider in order to identify his or her provider type, classification and/or area of specialization. Both provider identifiers and provider taxonomy.
Then the form is sent to the patient's medical insurance.Once the insurance receives the form, they review the charges, determine the patient's benefits, and pay out according to the negotiated rates.Unlike the CMS 1500 claim form, however, the UB-04 form includes a much more complicated set of boxes. These specify the types of services provided during the patient's hospital stay.They need to be filled out accurately to make sure that the claim is paid correctly the first time it gets sent. But how do you fill one out correctly?Filling out the formThe UB-04 claim form includes many of the same basic boxes as the CMS1500 claim form, including:. patient demographics. provider identification information.

What Does A Ub 92 Vs Hcfa 1500 Form Look Like On Math Plus
procedures and charges. insurance plan identification information.The top of the form includes an area for the provider information, including federal tax identification number. There's also a space for the patient's medical record number, which is assigned to the patient by the provider's office.Underneath this section, there's a small section on patient identifying information, and a section with boxes for occurrence dates and condition codes.These are a necessary part of hospital billing, because many people who are admitted and treated in the hospital have complicated, life-threatening conditions.The more information provided to the patient's insurance the better.
Blog
- Serial Number For T Bain
- Man With No Name Series
- Calculate Latency By Distance
- Easy Driver Pack Windows 7 32 Bit
- Anno 1701 Download Vollversion
- Fallout 4 Nexus Assault Carbine
- Pirates Of The Caribbean Full Movie
- Wallpaper Engine Download Themes
- Beyond The Reach Of The Invisible Hand, D.a. Yao Pdf
- Ultimate Windows Tweaker Italiano
- Best Mod For Rome 2
- Faire De La Vente De Billetterie Ne Ligne
- Euro Truck Simulator 2 Produktschlussel Generator
- Assassin's Creed 2 Google Drive
- Aplikasi Hadits Shahih Pc
- Gundam Seed Destiny Episode 40
- The Black Project Looch Rapidgator